
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular Risk/Epidemiology
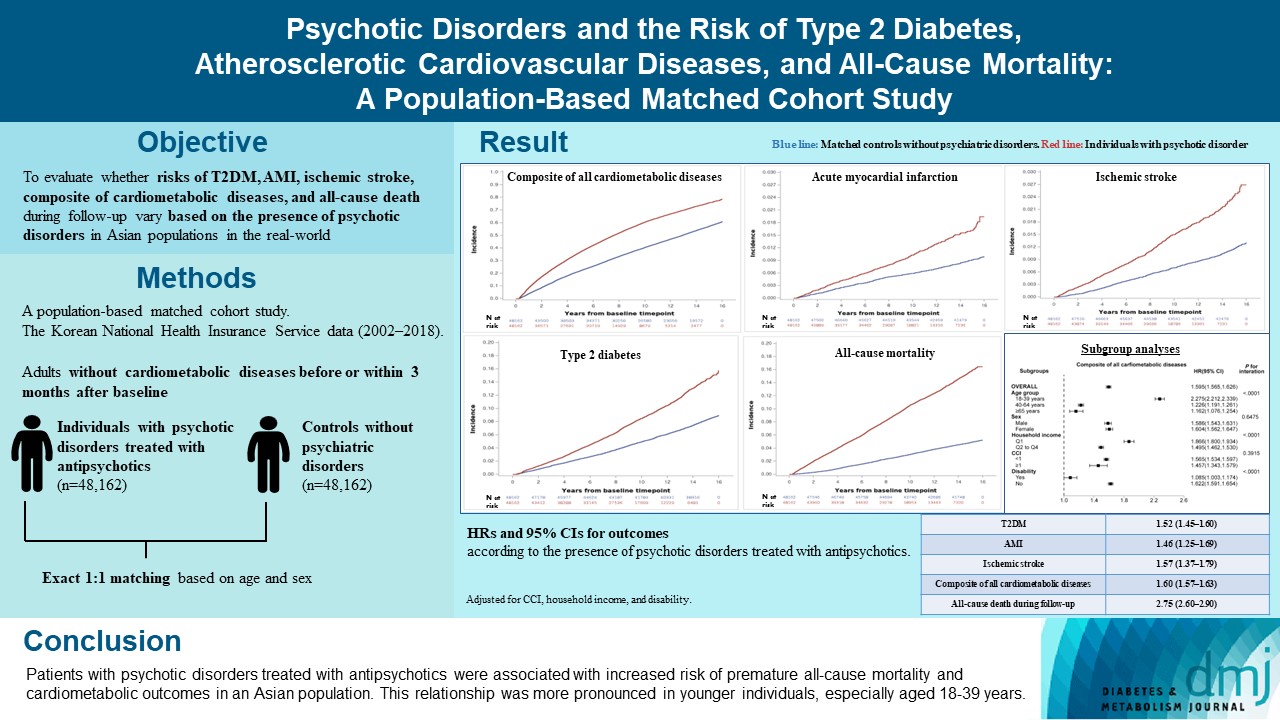
- Psychotic Disorders and the Risk of Type 2 Diabetes Mellitus, Atherosclerotic Cardiovascular Diseases, and All-Cause Mortality: A Population-Based Matched Cohort Study
- You-Bin Lee, Hyewon Kim, Jungkuk Lee, Dongwoo Kang, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim, Hong Jin Jeon, Kyu Yeon Hur
- Diabetes Metab J. 2024;48(1):122-133. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0431
- 1,089 View
- 144 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The effects of psychotic disorders on cardiometabolic diseases and premature death need to be determined in Asian populations.
Methods
In this population-based matched cohort study, the Korean National Health Insurance Service database (2002 to 2018) was used. The risk of type 2 diabetes mellitus (T2DM), acute myocardial infarction (AMI), ischemic stroke, composite of all cardiometabolic diseases, and all-cause death during follow-up was compared between individuals with psychotic disorders treated with antipsychotics (n=48,162) and 1:1 matched controls without psychiatric disorders among adults without cardiometabolic diseases before or within 3 months after baseline.
Results
In this cohort, 53,683 composite cases of all cardiometabolic diseases (during median 7.38 years), 899 AMI, and 1,216 ischemic stroke cases (during median 14.14 years), 7,686 T2DM cases (during median 13.26 years), and 7,092 deaths (during median 14.23 years) occurred. The risk of all outcomes was higher in subjects with psychotic disorders than matched controls (adjusted hazard ratios [95% confidence intervals]: 1.522 [1.446 to 1.602] for T2DM; 1.455 [1.251 to 1.693] for AMI; 1.568 [1.373 to 1.790] for ischemic stroke; 1.595 [1.565 to 1.626] for composite of all cardiometabolic diseases; and 2.747 [2.599 to 2.904] for all-cause mortality) during follow-up. Similar patterns of associations were maintained in subgroup analyses but more prominent in younger individuals (P for interaction <0.0001) when categorized as those aged 18–39, 40–64, or ≥65 years.
Conclusion
Patients with psychotic disorders treated with antipsychotics were associated with increased risk of premature allcause mortality and cardiometabolic outcomes in an Asian population. This relationship was more pronounced in younger individuals, especially aged 18 to 39 years.
- Complications
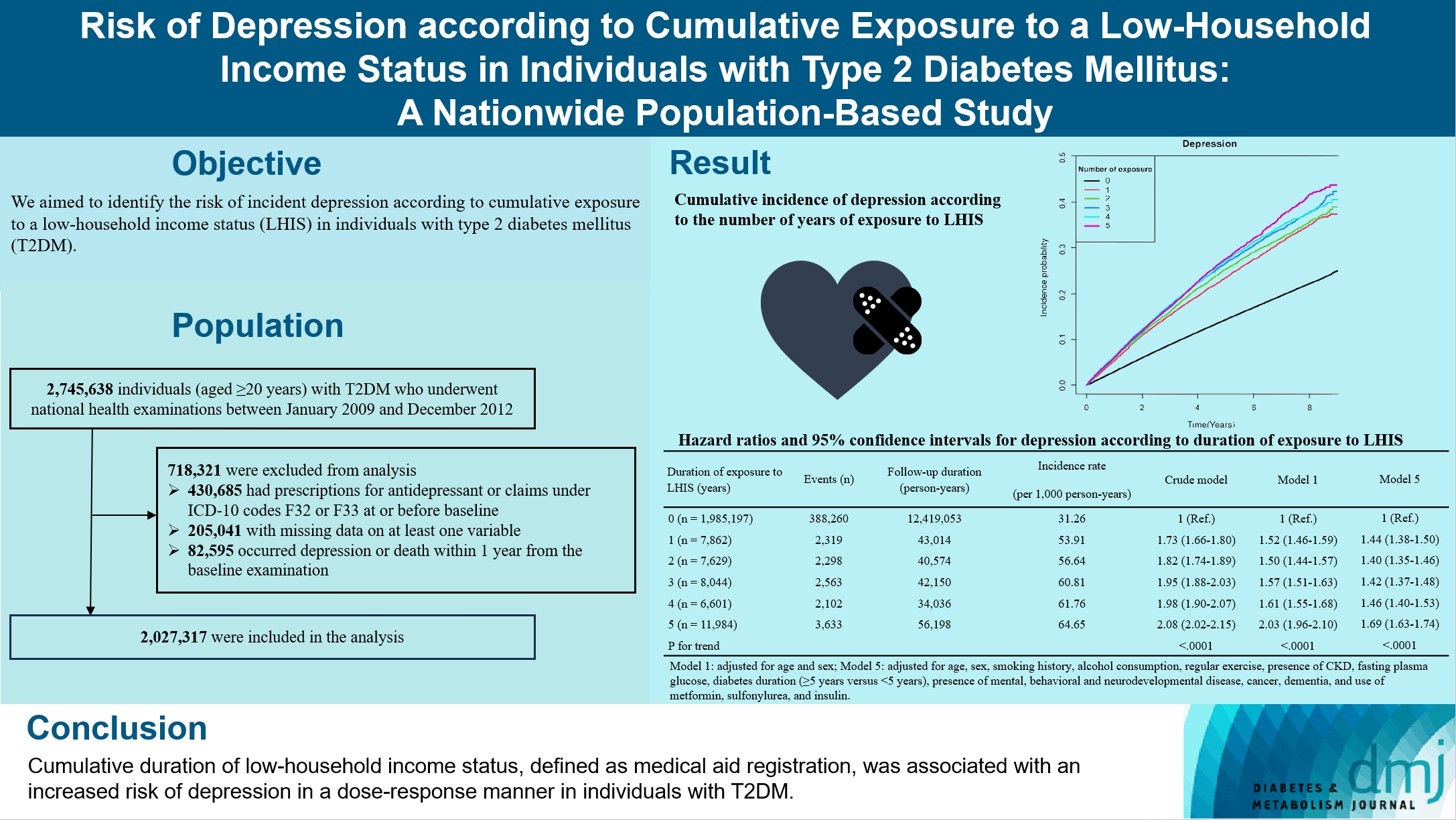
- Risk of Depression according to Cumulative Exposure to a Low-Household Income Status in Individuals with Type 2 Diabetes Mellitus: A Nationwide Population- Based Study
- So Hee Park, You-Bin Lee, Kyu-na Lee, Bongsung Kim, So Hyun Cho, So Yoon Kwon, Jiyun Park, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Kyungdo Han, Jae Hyeon Kim
- Diabetes Metab J. 2024;48(2):290-301. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0299
- 883 View
- 129 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We aimed to identify the risk of incident depression according to cumulative exposure to a low-household income status in individuals with type 2 diabetes mellitus (T2DM).
Methods
For this retrospective longitudinal population-based cohort study, we used Korean National Health Insurance Service data from 2002 to 2018. Risk of depression was assessed according to cumulative exposure to low-household income status (defined as Medical Aid registration) during the previous 5 years among adults (aged ≥20 years) with T2DM and without baseline depression who underwent health examinations from 2009 to 2012 (n=2,027,317).
Results
During an average 6.23 years of follow-up, 401,175 incident depression cases occurred. Advance in cumulative number of years registered for medical aid during the previous 5 years from baseline was associated with an increased risk of depression in a dose-dependent manner (hazard ratio [HR], 1.44 [95% confidence interval (CI), 1.38 to 1.50]; HR, 1.40 [95% CI, 1.35 to 1.46]; HR, 1.42, [95% CI, 1.37 to 1.48]; HR, 1.46, [95% CI, 1.40 to 1.53]; HR, 1.69, [95% CI, 1.63 to 1.74] in groups with 1 to 5 exposed years, respectively). Insulin users exposed for 5 years to a low-household income state had the highest risk of depression among groups categorized by insulin use and duration of low-household income status.
Conclusion
Cumulative duration of low-household income status, defined as medical aid registration, was associated with an increased risk of depression in a dose-response manner in individuals with T2DM.
- Metabolic Risk/Epidemiology
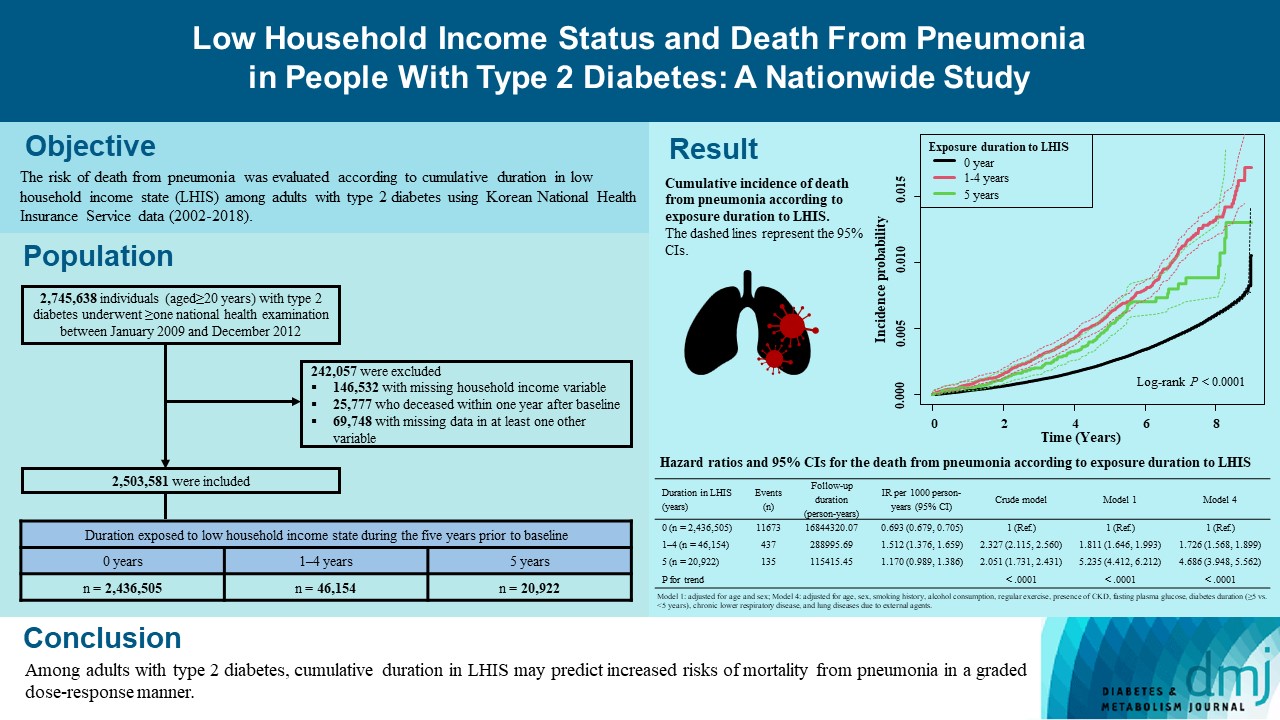
- Low Household Income Status and Death from Pneumonia in People with Type 2 Diabetes Mellitus: A Nationwide Study
- You-Bin Lee, So Hee Park, Kyu-na Lee, Bongsung Kim, So Yoon Kwon, Jiyun Park, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Kyungdo Han, Jae Hyeon Kim
- Diabetes Metab J. 2023;47(5):682-692. Published online June 22, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0184
- 1,584 View
- 121 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We explored the risk of death from pneumonia according to cumulative duration in low household income state (LHIS) among adults with type 2 diabetes mellitus (T2DM).
Methods
Using Korean National Health Insurance Service data (2002 to 2018), the hazards of mortality from pneumonia were analyzed according to duration in LHIS (being registered to Medical Aid) during the 5 years before baseline (0, 1–4, and 5 years) among adults with T2DM who underwent health examinations between 2009 and 2012 (n=2,503,581). Hazards of outcomes were also compared in six groups categorized by insulin use and duration in LHIS.
Results
During a median 7.18 years, 12,245 deaths from pneumonia occurred. Individuals who had been exposed to LHIS had higher hazards of death from pneumonia in a dose-response manner (hazard ratio [HR], 1.726; 95% confidence interval [CI], 1.568 to 1.899 and HR, 4.686; 95% CI, 3.948 to 5.562 in those exposed for 1–4 and 5 years, respectively) compared to the non-exposed reference. Insulin users exposed for 5 years to LHIS exhibited the highest outcome hazard among six groups categorized by insulin use and duration in LHIS.
Conclusion
Among adults with T2DM, cumulative duration in LHIS may predict increased risks of mortality from pneumonia in a graded dose-response manner. Insulin users with the longest duration in LHIS might be the group most vulnerable to death from pneumonia among adults with T2DM.
- Guideline/Fact Sheet
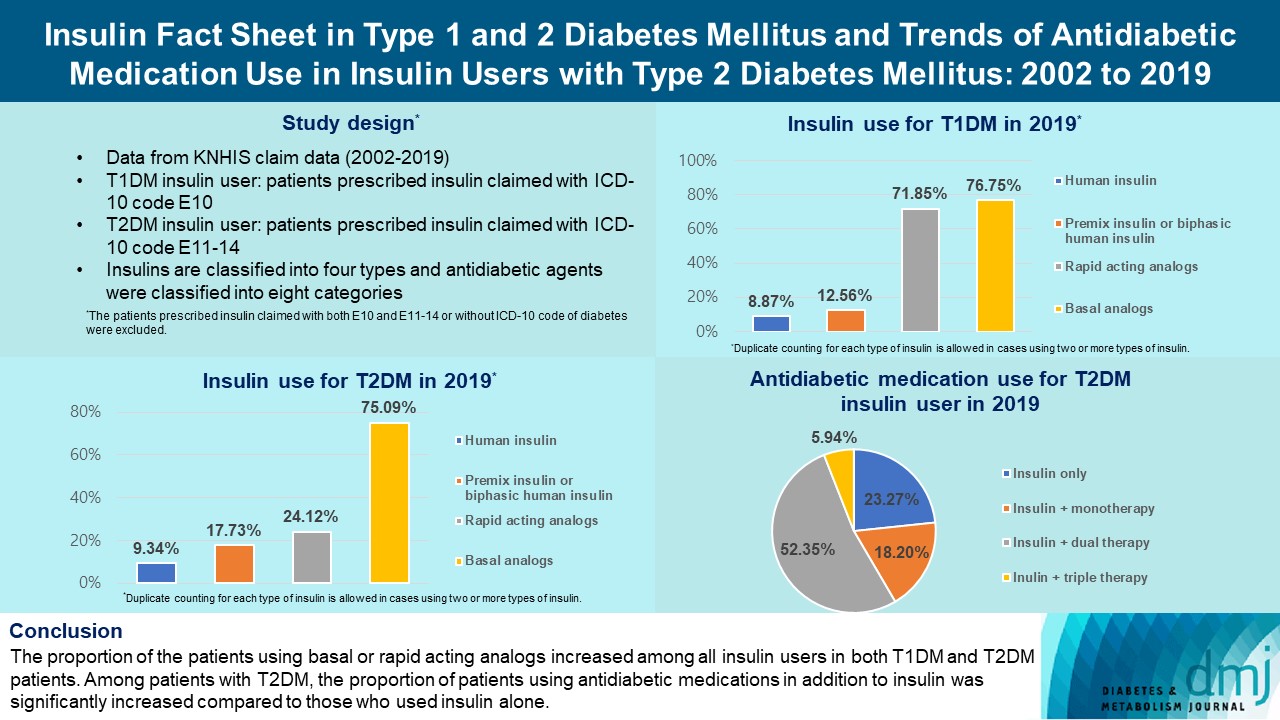
- Insulin Fact Sheet in Type 1 and 2 Diabetes Mellitus and Trends of Antidiabetic Medication Use in Insulin Users with Type 2 Diabetes Mellitus: 2002 to 2019
- Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
- Diabetes Metab J. 2023;47(2):211-219. Published online February 7, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0346
- 3,535 View
- 258 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the trends of insulin use among Korean patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM). Changes in prescription of antidiabetic medications in T2DM patients taking insulin therapy were evaluated.
Methods
We analyzed data from the National Health Insurance Service database in Korea to evaluate the prevalence of insulin users and trends of insulin use in T1DM and T2DM patients from January 2002 to December 2019. We also investigated numbers and types of antidiabetic medications in insulin users with T2DM.
Results
The overall total number of insulin users increased from 2002 to 2019, reaching 348,254 for T2DM and 20,287 for T1DM in 2019 compared with 109,974 for T2DM and 34,972 for T1DM in 2002. The proportion of patients using basal analogs and short acting analogs have increased and those using human insulin, premixed insulin, or biphasic human insulin have decreased (rapid acting analogs: 71.85% and 24.12% in T1DM and T2DM, respectively, in 2019; basal analogs: 76.75% and 75.09% in T1DM and T2DM, respectively, in 2019). The use of other antidiabetic medication in addition to insulin increased for T2DM, especially in dual therapy, reaching up to 52.35% in 2019 compared with 16.72% in 2002.
Conclusion
The proportion of the patients using basal or rapid acting analogs increased among all insulin users in both T1DM and T2DM patients. Among patients with T2DM, the proportion of patients using antidiabetic medications in addition to insulin was significantly increased compared to those who used insulin alone. -
Citations
Citations to this article as recorded by- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
Ji Yoon Kim, Sang-Man Jin, Sarah B. Andrade, Boyang Chen, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Evaluation of pharmacokinetic interactions between lobeglitazone, empagliflozin, and metformin in healthy subjects
Heeyoung Kim, Choon Ok Kim, Hyeonsoo Park, Min Soo Park, Dasohm Kim, Taegon Hong, Yesong Shin, Byung Hak Jin
Translational and Clinical Pharmacology.2023; 31(1): 59. CrossRef - Smart Insulin Pen: Managing Insulin Therapy for People with Diabetes in the Digital Era
Jee Hee Yoo, Jae Hyeon Kim
The Journal of Korean Diabetes.2023; 24(4): 190. CrossRef
- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
- Association between Metabolic Syndrome and Microvascular Complications in Chinese Adults with Type 1 Diabetes Mellitus (Diabetes Metab J 2022;46:93-103)
- Gyuri Kim
- Diabetes Metab J. 2022;46(3):512-514. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0134
- 2,703 View
- 119 Download
- 2 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Receiver Operator Characteristic (ROC) Analysis of Lipids, Proteins, DNA Oxidative Damage, and Antioxidant Defense in Plasma and Erythrocytes of Young Reproductive-Age Men with Early Stages of Type 1 Diabetes Mellitus (T1DM) Nephropathy in the Irkutsk Reg
Marina Darenskaya, Elena Chugunova, Sergey Kolesnikov, Natalya Semenova, Isay Michalevich, Olga Nikitina, Anastasya Lesnaya, Lyubov Kolesnikova
Metabolites.2022; 12(12): 1282. CrossRef - Recent advances and potentiality of postbiotics in the food industry: Composition, inactivation methods, current applications in metabolic syndrome, and future trends
Yujie Zhong, Tao Wang, Ruilin Luo, Jiayu Liu, Ruyi Jin, Xiaoli Peng
Critical Reviews in Food Science and Nutrition.2022; : 1. CrossRef
- Receiver Operator Characteristic (ROC) Analysis of Lipids, Proteins, DNA Oxidative Damage, and Antioxidant Defense in Plasma and Erythrocytes of Young Reproductive-Age Men with Early Stages of Type 1 Diabetes Mellitus (T1DM) Nephropathy in the Irkutsk Reg
- Technology/Device
- A 4-Week, Two-Center, Open-Label, Single-Arm Study to Evaluate the Safety and Efficacy of EOPatch in Well-Controlled Type 1 Diabetes Mellitus
- Jiyun Park, Nammi Park, Sangjin Han, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Woo Je Lee, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(6):941-947. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0299
- 5,171 View
- 269 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study evaluated the safety and efficacy of tubeless patch pump called EOPatch in patients with well-controlled type 1 diabetes mellitus (T1DM). This 4-week, two-center, open-label, single-arm study enrolled 10 adult patients diagnosed with T1DM with glycosylated hemoglobin less than 7.5%. The co-primary end points were patch pump usage time for one attachment and number of serious adverse events related to the patch pump. The secondary end points were total amount of insulin injected per patch and changes in glycemic parameters including continuous glucose monitoring data compared to those at study entry. The median usage time per patch was 84.00 hours (interquartile range, 64.50 to 92.50). Serious adverse events did not occur during the trial. Four weeks later, time in range 70 to 180 mg/dL was significantly improved (70.71%±17.14 % vs. 82.96%±9.14%, P=0.01). The times spent below range (<54 mg/dL) and above range (>180 mg/dL) also improved (All P<0.05). Four-week treatment with a tubeless patch pump was safe and led to clinical improvement in glycemic control.
-
Citations
Citations to this article as recorded by- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
Qian Yang, Zebo Zhang, Junshu Lin, Boyu Zhu, Rongying Yu, Xinru Li, Bin Su, Bo Zhao
ELECTROPHORESIS.2024; 45(5-6): 433. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - A true continuous healthcare system for type 1 diabetes
Jiyong Kim, Salman Khan, Eun Kyu Kim, Hye-Jun Kil, Bo Min Kang, Hyo Geon Lee, Jin-Woo Park, Jun Young Yoon, Woochul Kim
Nano Energy.2023; 113: 108553. CrossRef
- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
- Technology/Device
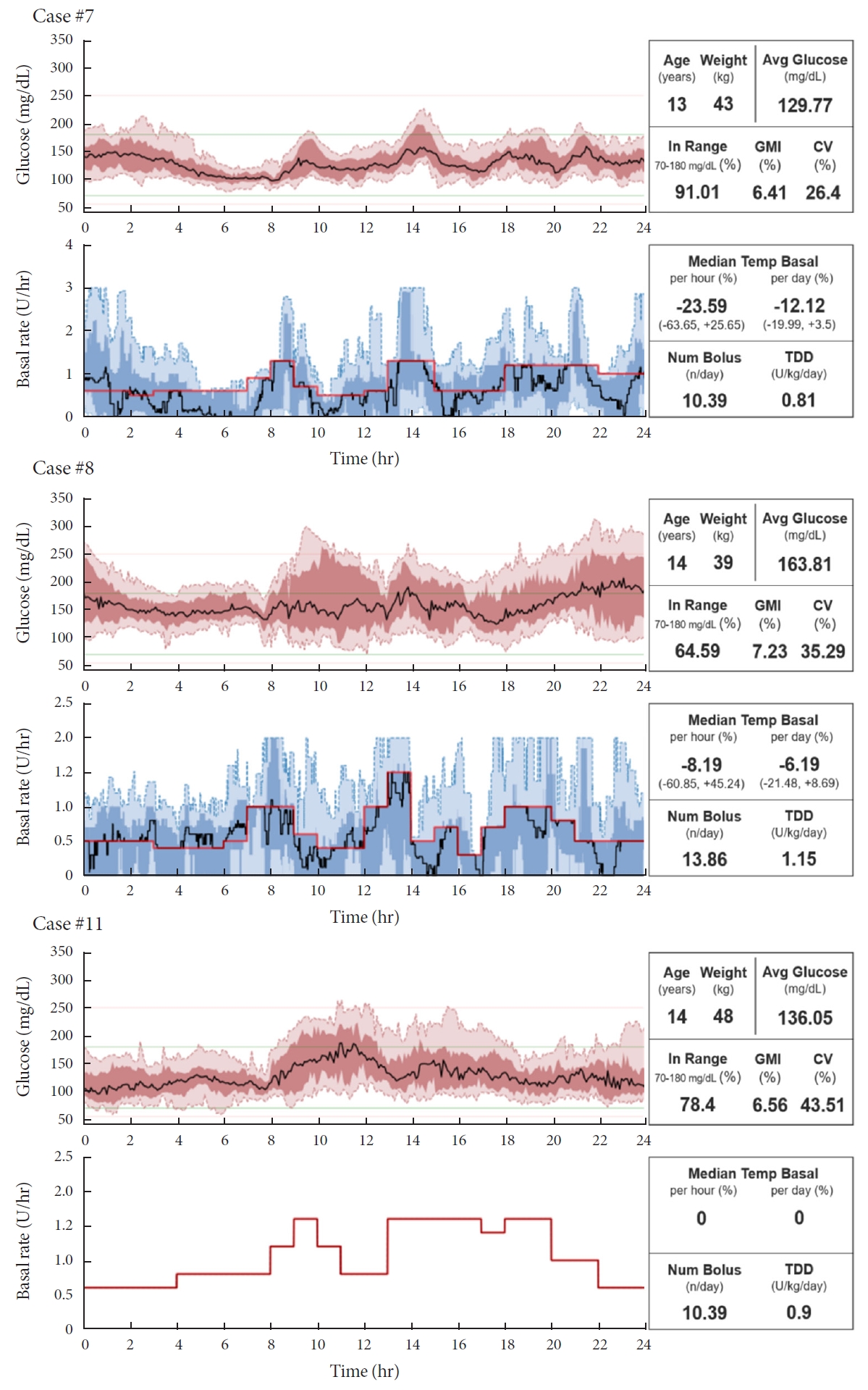
- Do-It-Yourself Open Artificial Pancreas System in Children and Adolescents with Type 1 Diabetes Mellitus: Real-World Data
- Min Sun Choi, Seunghyun Lee, Jiwon Kim, Gyuri Kim, Sung Min Park, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(1):154-159. Published online November 23, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0011
- 5,295 View
- 192 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Few studies have been conducted among Asian children and adolescents with type 1 diabetes mellitus (T1DM) using do-it-yourself artificial pancreas system (DIY-APS). We evaluated real-world data of pediatric T1DM patients using DIY-APS. Data were obtained for 10 patients using a DIY-APS with algorithms. We collected sensor glucose and insulin delivery data from each participant for a period of 4 weeks. Average glycosylated hemoglobin was 6.2%±0.3%. The mean percentage of time that glucose level remained in the target range of 70 to 180 mg/dL was 82.4%±7.8%. Other parameters including time above range, time below range and mean glucose were also within the recommended level, similar to previous commercial and DIY-APS studies. However, despite meeting the target range, unadjusted gaps were still observed between the median basal setting and temporary basal insulin, which should be handled by healthcare providers.
-
Citations
Citations to this article as recorded by- Advances in Continuous Glucose Monitoring and Integrated Devices for Management of Diabetes with Insulin-Based Therapy: Improvement in Glycemic Control
Jee Hee Yoo, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(1): 27. CrossRef - Open-source automated insulin delivery systems (OS-AIDs) in a pediatric population with type 1 diabetes in a real-life setting: the AWeSoMe study group experience
Judith Nir, Marianna Rachmiel, Abigail Fraser, Yael Lebenthal, Avivit Brener, Orit Pinhas-Hamiel, Alon Haim, Eve Stern, Noa Levek, Tal Ben-Ari, Zohar Landau
Endocrine.2023; 81(2): 262. CrossRef - Efficacy and safety of Android artificial pancreas system use at home among adults with type 1 diabetes mellitus in China: protocol of a 26-week, free-living, randomised, open-label, two-arm, two-phase, crossover trial
Mengyun Lei, Beisi Lin, Ping Ling, Zhigu Liu, Daizhi Yang, Hongrong Deng, Xubin Yang, Jing Lv, Wen Xu, Jinhua Yan
BMJ Open.2023; 13(8): e073263. CrossRef - Barriers to Uptake of Open-Source Automated Insulin Delivery Systems: Analysis of Socioeconomic Factors and Perceived Challenges of Caregivers of Children and Adolescents With Type 1 Diabetes From the OPEN Survey
Antonia Huhndt, Yanbing Chen, Shane O’Donnell, Drew Cooper, Hanne Ballhausen, Katarzyna A. Gajewska, Timothée Froment, Mandy Wäldchen, Dana M. Lewis, Klemens Raile, Timothy C. Skinner, Katarina Braune
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - Toward Personalized Hemoglobin A1c Estimation for Type 2 Diabetes
Namho Kim, Da Young Lee, Wonju Seo, Nan Hee Kim, Sung-Min Park
IEEE Sensors Journal.2022; 22(23): 23023. CrossRef
- Advances in Continuous Glucose Monitoring and Integrated Devices for Management of Diabetes with Insulin-Based Therapy: Improvement in Glycemic Control
- Cardiovascular Risk/Epidemiology
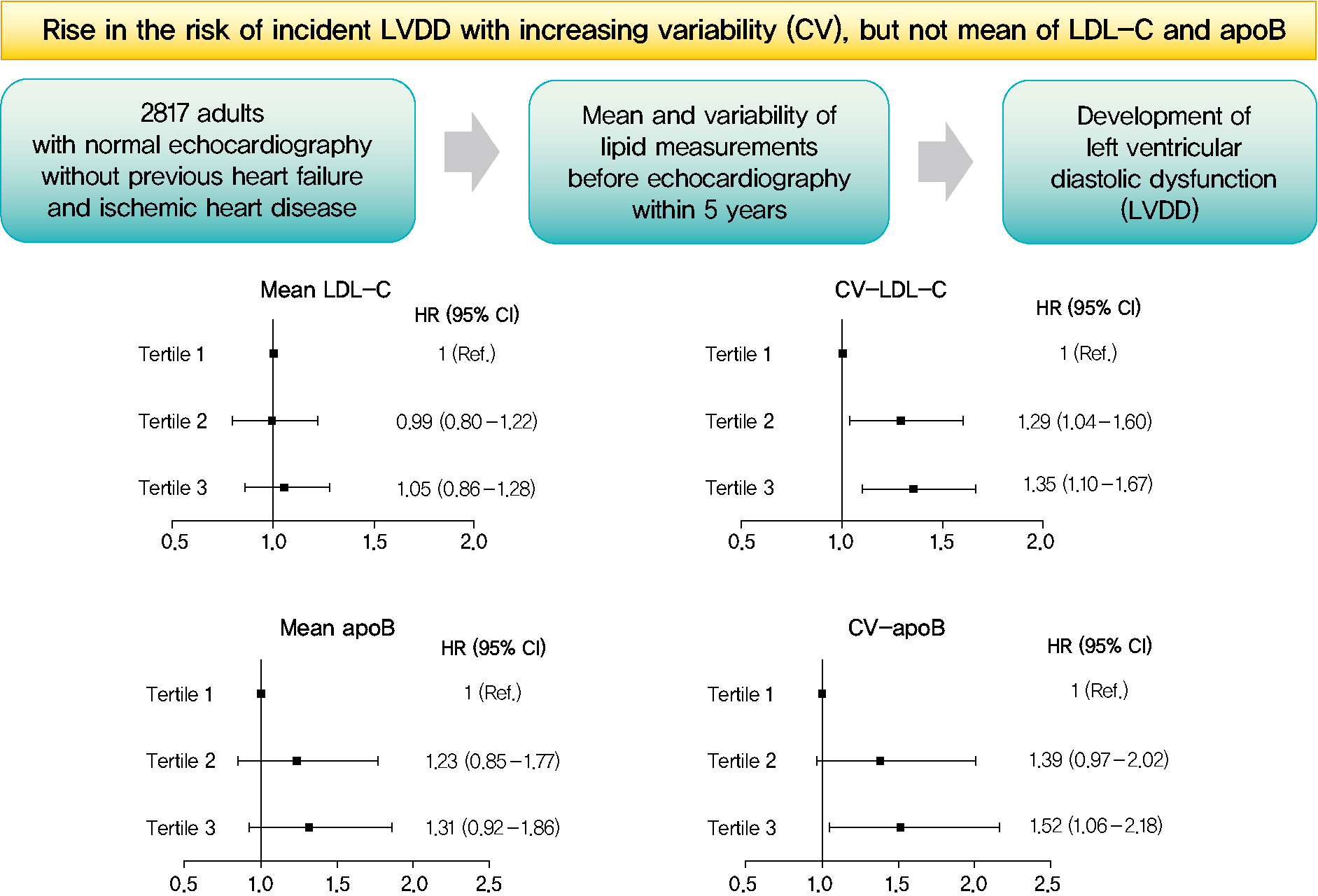
- Mean and Variability of Lipid Measurements and Risk for Development of Subclinical Left Ventricular Diastolic Dysfunction
- Jiyun Park, Mira Kang, Jiyeon Ahn, Min Young Kim, Min Sun Choi, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Jae Hyeon Kim, Jeong Hoon Yang, Sang-Man Jin
- Diabetes Metab J. 2022;46(2):286-296. Published online November 22, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0080
- 5,661 View
- 196 Download
- 1 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 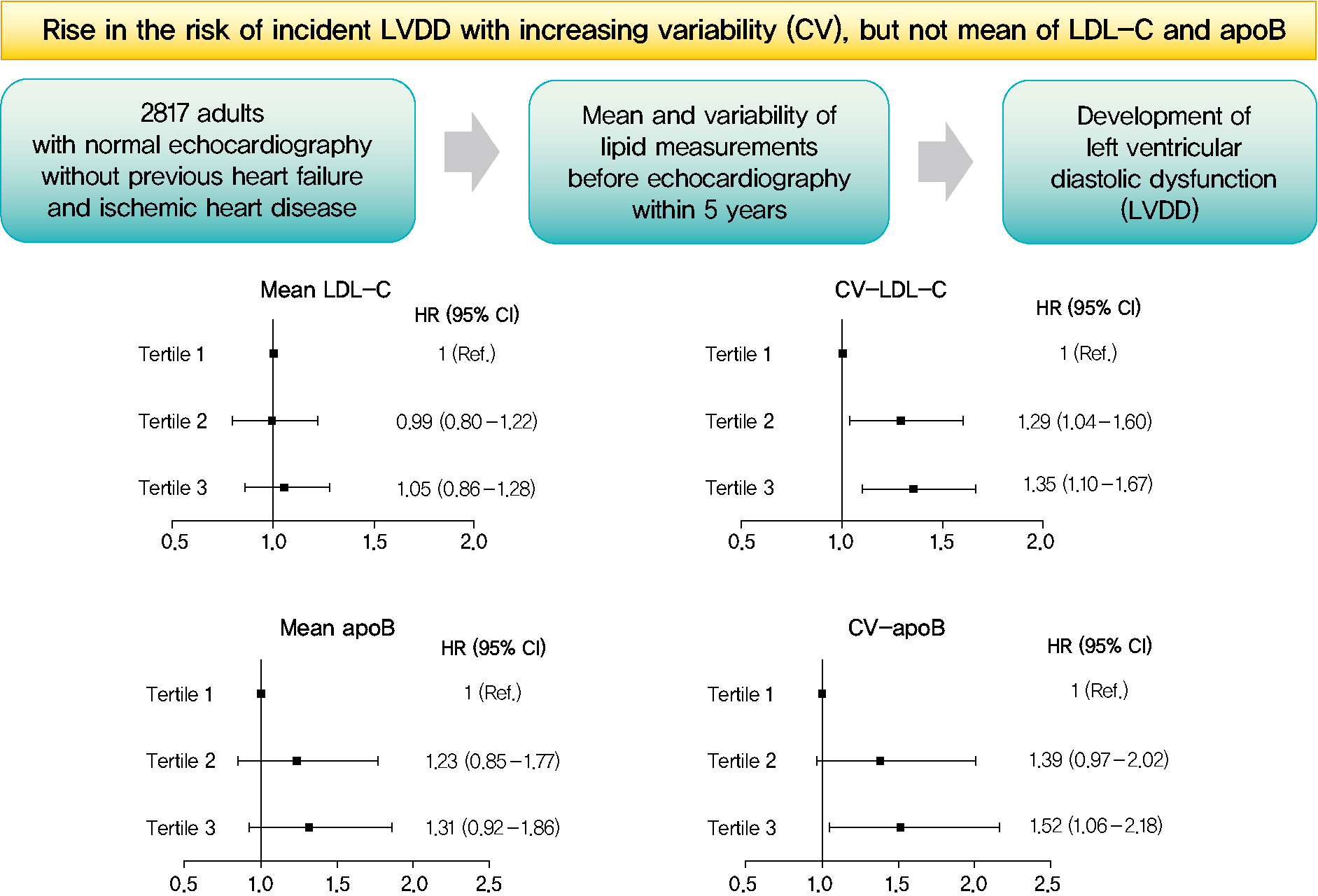
- Background
Subclinical left ventricular diastolic dysfunction (LVDD) is an emerging consequence of increased insulin resistance, and dyslipidemia is one of the few correctable risk factors of LVDD. This study evaluated the role of mean and visit-to-visit variability of lipid measurements in risk of LVDD in a healthy population.
Methods
This was a 3.7-year (interquartile range, 2.1 to 4.9) longitudinal cohort study including 2,817 adults (median age 55 years) with left ventricular ejection fraction >50% who underwent an annual or biannual health screening between January 2008 and July 2016. The mean, standard deviation (SD), coefficient of variation (CV), variability independent of the mean (VIM), and average real variability of total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), apolipoprotein B (apoB), non-HDL-C, and triglycerides were obtained from three to six measurements during the 5 years preceding the first echocardiogram.
Results
Among the 2,817 patients, 560 (19.9%) developed LVDD. The mean of no component of lipid measurements was associated with risk of LVDD. CV (hazard ratio [HR], 1.35; 95% confidence interval [CI], 1.10 to 1.67), SD (HR, 1.27; 95% CI, 1.03 to 1.57), and VIM (HR, 1.26; 95% CI, 1.03 to 1.55) of LDL-C and all the variability parameters of apoB were significantly associated with development of LVDD. The association between CV-LDL and risk of LVDD did not have significant interaction with sex, increasing/decreasing trend at baseline, or use of stain and/or lipid-modifying agents.
Conclusion
The variability of LDL-C and apoB, rather than their mean, was associated with risk for LVDD. -
Citations
Citations to this article as recorded by- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
Jinqi Wang, Rui Jin, Xiaohan Jin, Zhiyuan Wu, Haiping Zhang, Ze Han, Zongkai Xu, Yueruijing Liu, Xiaoyu Zhao, Xiuhua Guo, Lixin Tao
Journal of the American Heart Association.2023;[Epub] CrossRef - Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
Hye Jin Yoo
Diabetes & Metabolism Journal.2022; 46(2): 257. CrossRef
- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
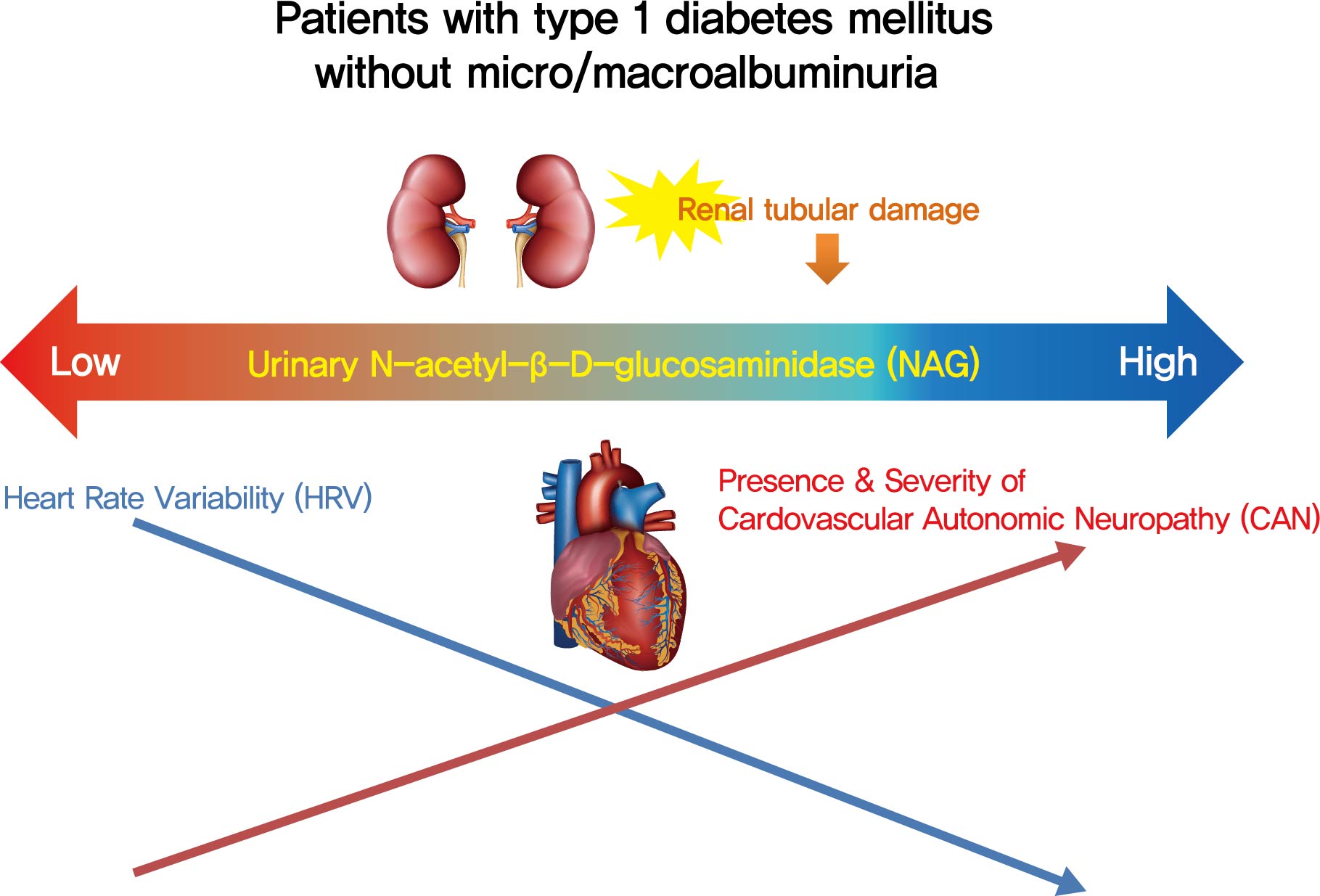
- Complications
- Association of Urinary N-Acetyl-β-D-Glucosaminidase with Cardiovascular Autonomic Neuropathy in Type 1 Diabetes Mellitus without Nephropathy
- Min Sun Choi, Ji Eun Jun, Sung Woon Park, Jee Hee Yoo, Jiyeon Ahn, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
- Diabetes Metab J. 2021;45(3):349-357. Published online February 2, 2021
- DOI: https://doi.org/10.4093/dmj.2019.0211
- 5,630 View
- 121 Download
- 1 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 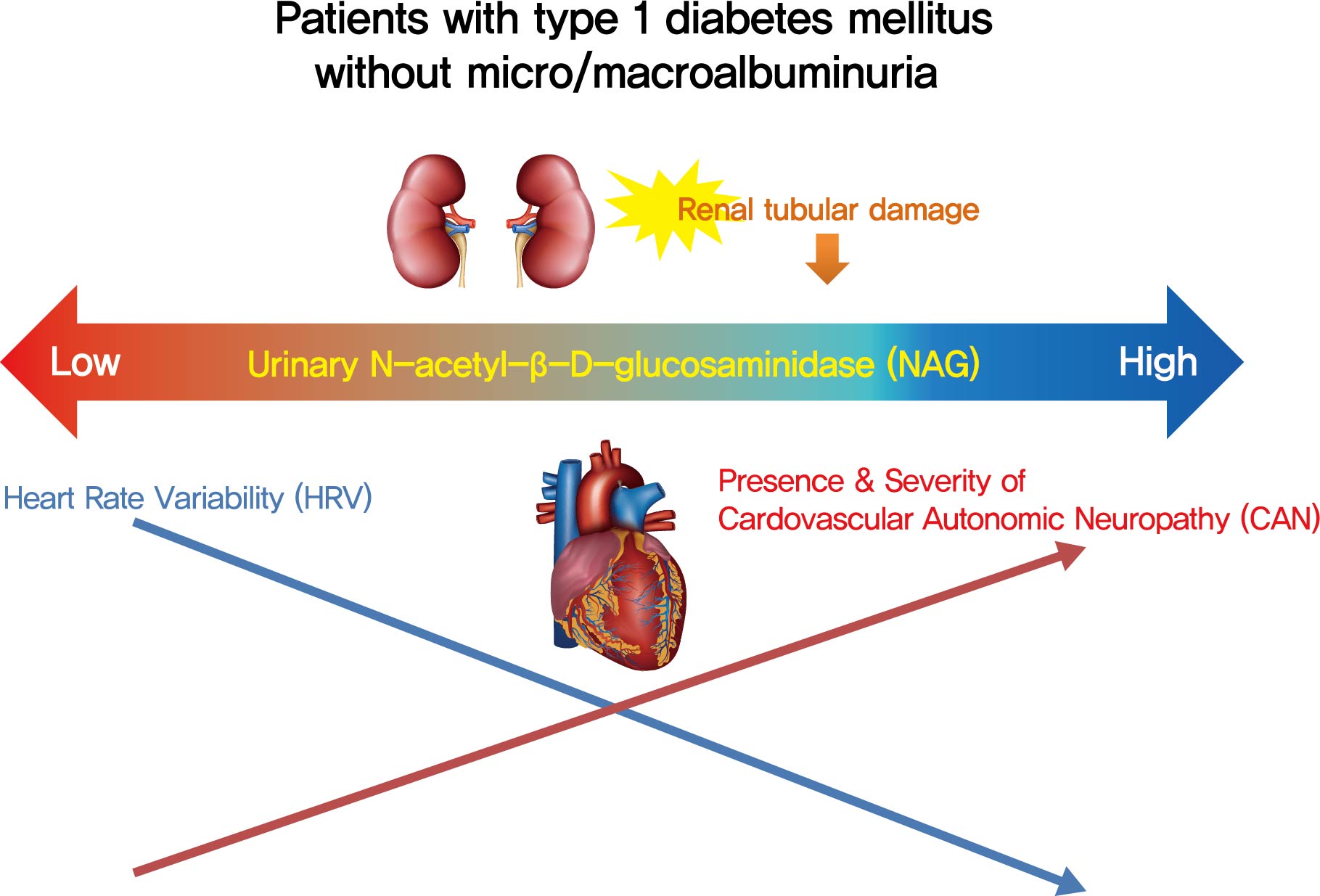
- Background
Cardiovascular autonomic neuropathy (CAN) is a common microvascular complication of diabetes and related to albuminuria in diabetic nephropathy (DN). Urinary N-acetyl-β-D-glucosaminidase (uNAG) is a renal tubular injury marker which has been reported as an early marker of DN even in patients with normoalbuminuria. This study evaluated whether uNAG is associated with the presence and severity of CAN in patients with type 1 diabetes mellitus (T1DM) without nephropathy.
Methods
This cross-sectional study comprised 247 subjects with T1DM without chronic kidney disease and albuminuria who had results for both uNAG and autonomic function tests within 3 months. The presence of CAN was assessed by age-dependent reference values for four autonomic function tests. Total CAN score was assessed as the sum of the partial points of five cardiovascular reflex tests and was used to estimatethe severity of CAN. The correlations between uNAG and heart rate variability (HRV) parameters were analyzed.
Results
The association between log-uNAG and presence of CAN was significant in a multivariate logistic regression model (adjusted odds ratio, 2.39; 95% confidence interval [CI], 1.08 to 5.28; P=0.031). Total CAN score was positively associated with loguNAG (β=0.261, P=0.026) in the multivariate linear regression model. Log-uNAG was inversely correlated with frequency-domain and time-domain indices of HRV.
Conclusion
This study verified the association of uNAG with presence and severity of CAN and changes in HRV in T1DM patients without nephropathy. The potential role of uNAG should be further assessed for high-risk patients for CAN in T1DM patients without nephropathy. -
Citations
Citations to this article as recorded by- Determination of Diabetes-associated Cardiovascular Autonomic Neuropathy Risk Factors among Insulin and Non-insulin Dependent Diabetics
Ibrahim Abdulsada, Zain Alabdeen Obaid, Farah Almerza, Mays Alwaeli, Anmar Al-Elayawi, Taha Al-Dayyeni, Harir Al-Tuhafy
The Journal of Medical Research.2023; 9(6): 141. CrossRef - Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef
- Determination of Diabetes-associated Cardiovascular Autonomic Neuropathy Risk Factors among Insulin and Non-insulin Dependent Diabetics
- Type 1 Diabetes
- Age at Diagnosis and the Risk of Diabetic Nephropathy in Young Patients with Type 1 Diabetes Mellitus
- Jong Ha Baek, Woo Je Lee, Byung-Wan Lee, Soo Kyoung Kim, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim
- Diabetes Metab J. 2021;45(1):46-54. Published online July 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0134

- 6,802 View
- 230 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background The aim of this study was to evaluate characteristics and risk of diabetic complications according to age at diagnosis among young adults with type 1 diabetes mellitus (T1DM).
Methods A total of 255 T1DM patients aged less than 40 years were included. Patients were categorized into three groups (<20, 20 to 29, and 30 to 40 years) according to age at diagnosis. Diabetic nephropathy (DN) was defined when spot urine-albumin creatinine ratio was 300 mg/g or more and/or estimated glomerular filtration ratio (eGFR) level was 60 mL/min/1.73 m2 or less.
Results Median age at diagnosis was 25 years and disease duration was 14 years. Individuals diagnosed with T1DM at childhood/adolescent (age <20 years) had lower stimulated C-peptide levels. They received more intensive insulin treatment with higher total daily insulin doses compared to older onset groups. The prevalence of DN was higher in the childhood/adolescent-onset group than in older onset groups (25.3% vs. 15.3% vs. 9.6%,
P =0.022). The eGFR was inversely associated with disease duration whilst the degree of decrease was more prominent in the childhood/adolescent-onset group than in the later onset group (aged 30 to 40 years;P <0.001). Childhood/adolescent-onset group was independently associated with the risk of DN compared to the older onset group (aged 30 to 40 years; odds ratio, 3.47; 95% confidence interval, 1.45 to 8.33;P =0.005).Conclusion In individuals with childhood/adolescent-onset T1DM, the reduction in renal function is more prominent with disease duration. Early age-onset T1DM is an independent risk of DN.
-
Citations
Citations to this article as recorded by- Age at onset of type 1 diabetes between puberty and 30 years old is associated with increased diabetic nephropathy risk
Yen-Bo Lin, Wayne Huey-Herng Sheu, Su-Huey Lo, Yen-Po Yeh, Chien-Ning Huang, Chii-Min Hwu, Chang-Hsun Hsieh, Horng-Yi Ou, Lee-Ming Chuang, Jung-Fu Chen, Yu-Cheng Chen, Yun-Hsing Peng, Szu-Tah Chen, Shang-Ren Hsu, Yi-Ling Hsieh, Chih-Hsun Chu, Chieg-Hsiang
Scientific Reports.2024;[Epub] CrossRef - Targeted mapping and utilization of the perihepatic surface for therapeutic beta cell replacement and retrieval in diabetic non-human primates
David J. Leishman, Scott H. Oppler, Laura L. Hocum Stone, Timothy D. O’Brien, Sabarinathan Ramachandran, Bradley J. Willenberg, Andrew B. Adams, Bernhard J. Hering, Melanie L. Graham
Frontiers in Transplantation.2024;[Epub] CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - Continuous glucose monitoring with structured education in adults with type 2 diabetes managed by multiple daily insulin injections: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Kang Hee Sim, Bo-Yeon Kim, Jae Hyoung Cho, Jun Sung Moon, Soo Lim, Eun Seok Kang, Cheol-Young Park, Sin Gon Kim, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - Network-based identification and prioritization of key transcriptional factors of diabetic kidney disease
Ikhlak Ahmed, Mubarak Ziab, Sahar Da’as, Waseem Hasan, Sujitha P. Jeya, Elbay Aliyev, Sabah Nisar, Ajaz A. Bhat, Khalid Adnan Fakhro, Ammira S. Alshabeeb Akil
Computational and Structural Biotechnology Journal.2023; 21: 716. CrossRef - Comparison of diabetes distress and depression screening results of emerging adults with type 1 diabetes onset at different ages: findings from the German early-onset T1D study and the German Diabetes Study (GDS)
Anna Stahl-Pehe, Christina Bächle, Kálmán Bódis, Oana-Patricia Zaharia, Karin Lange, Reinhard W. Holl, Michael Roden, Joachim Rosenbauer, M. Roden, H. Al-Hasani, B Belgardt, GJ. Bönhof, V Burkart, A. E. Buyken, G. Geerling, C. Herder, A. Icks, K. Jandelei
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Hemoperfusion and functional state of the macula after simultaneous pancreas and kidney transplantation
IV Vorobyeva, EV Bulava, LK Moshetova, AV Pinchuk
Bulletin of Russian State Medical University.2022;[Epub] CrossRef - Sigesbeckia orientalis Extract Ameliorates the Experimental Diabetic Nephropathy by Downregulating the Inflammatory and Oxidative Stress Signaling Pathways
Chung-Ming Chen, Jer-Yiing Houng, Tsui-Ling Ko, Shu-Hui Juan, Hsiu-Chu Chou, Xing Li
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Impact of low-protein diet on cardiovascular risk factors and kidney function in diabetic nephropathy: A systematic review and meta-analysis of randomized-controlled trials
Mohammad Hassan Sohouli, Parvin Mirmiran, Shaikh Sanjid Seraj, Emad Kutbi, Hadil Ali Mohammed Alkahmous, Faisal Almuqayyid, Omar Ahnaf Arafah, Abdul Rahman Riad Barakeh, Ahmed Abu-Zaid
Diabetes Research and Clinical Practice.2022; 191: 110068. CrossRef - Age at Diagnosis and the Risk of Diabetic Nephropathy in Young Patients with Type 1 Diabetes Mellitus (Diabetes Metab J 2021;45:46-54)
Jong Ha Baek, Jae Hyeon Kim
Diabetes & Metabolism Journal.2021; 45(2): 281. CrossRef - Age at Diagnosis and the Risk of Diabetic Nephropathy in Young Patients with Type 1 Diabetes Mellitus (Diabetes Metab J 2021;45:46-54)
Ye Seul Yang, Tae Seo Sohn
Diabetes & Metabolism Journal.2021; 45(2): 277. CrossRef - Role of magnetic resonance diffusion weighted imaging in diagnosis of diabetic nephropathy in children living with type 1 diabetes mellitus
Eman Nabil Wahba, Ashraf Elsharkawy, Mohammad Hosny Awad, Ashraf Abdel Rahman, Amr Sarhan
Journal of Pediatric Endocrinology and Metabolism.2021; 34(12): 1585. CrossRef
- Age at onset of type 1 diabetes between puberty and 30 years old is associated with increased diabetic nephropathy risk
- Response: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (
Diabetes Metab J 2020;44:267–76) - Hokyou Lee, Gyuri Kim, Yong-ho Lee
- Diabetes Metab J. 2020;44(3):486-487. Published online June 29, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0127
- [Original]
- 3,901 View
- 51 Download
- 1 Crossref
-
 PDF
PDF PubReader
PubReader -
Citations
Citations to this article as recorded by- Association of Metabolic Dysfunction-Associated Fatty Liver Disease With Left Ventricular Diastolic Function and Cardiac Morphology
Dandan Peng, Zhenqiu Yu, Mingwei Wang, Junping Shi, Lei Sun, Yuanyuan Zhang, Wenbin Zhao, Chen Chen, Jiake Tang, Chunyi Wang, Jie Ni, Wen Wen, Jingjie Jiang
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Association of Metabolic Dysfunction-Associated Fatty Liver Disease With Left Ventricular Diastolic Function and Cardiac Morphology
- Metabolic Risk/Epidemiology
- Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus
- Hokyou Lee, Gyuri Kim, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
- Diabetes Metab J. 2020;44(2):267-276. Published online February 28, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0001
- 6,871 View
- 150 Download
- 25 Web of Science
- 27 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Impaired diastolic heart function has been observed in persons with non-alcoholic fatty liver disease (NAFLD) and/or with type 2 diabetes mellitus (T2DM). However, it is unclear whether NAFLD fibrotic progression, i.e., non-alcoholic steatohepatitis, poses an independent risk for diastolic dysfunction in T2DM. We investigated the association between liver fibrosis and left ventricular (LV) diastolic dysfunction in T2DM.
Methods We analyzed 606 patients with T2DM, aged ≥50 years, who had undergone liver ultrasonography and pulsed-wave Doppler echocardiography. Insulin sensitivity was measured by short insulin tolerance test. Presence of NAFLD and/or advanced liver fibrosis was determined by abdominal ultrasonography and NAFLD fibrosis score (NFS). LV diastolic dysfunction was defined according to transmitral peak early to late ventricular filling (E/A) ratio and deceleration time, using echocardiography.
Results LV diastolic dysfunction was significantly more prevalent in the NAFLD versus non-NAFLD group (59.7% vs. 49.0%,
P =0.011). When NAFLD was stratified by NFS, subjects with advanced liver fibrosis exhibited a higher prevalence of diastolic dysfunction (49.0%, 50.7%, 61.8%; none, simple steatosis, advanced fibrosis, respectively;P for trend=0.003). In multivariable logistic regression, liver fibrosis was independently associated with diastolic dysfunction (odds ratio [OR], 1.58; 95% confidence interval [CI], 1.07 to 2.34;P =0.022) after adjusting for insulin resistance and cardiometabolic risk factors. This association remained significant in patients without insulin resistance (OR, 4.32; 95% CI, 1.73 to 11.51;P =0.002).Conclusions Liver fibrosis was associated with LV diastolic dysfunction in patients with T2DM and may be an independent risk factor for diastolic dysfunction, especially in patients without systemic insulin resistance.
-
Citations
Citations to this article as recorded by- Anti-hepatopathy and anti-nephropathy activities of Taraxacum officinale in a rat model of Streptozotocin diabetes-induced hepatorenal toxicity and dyslipidemia via attenuation of oxidative stress, inflammation, apoptosis, electrolyte imbalances, and mito
Sunday Aderemi Adelakun, Aniah Julius Akomaye, Olusegun Dare Omotoso, Olukayode Abimbola Arowosegbe
Aspects of Molecular Medicine.2024; 3: 100034. CrossRef - Epidemiology of heart failure in diabetes: a disease in disguise
Anna G. Hoek, Elisa Dal Canto, Eva Wenker, Navin Bindraban, M. Louis Handoko, Petra J. M. Elders, Joline W. J. Beulens
Diabetologia.2024; 67(4): 574. CrossRef - NASH triggers cardiometabolic HFpEF in aging mice
Dániel Kucsera, Mihály Ruppert, Nabil V. Sayour, Viktória E. Tóth, Tamás Kovács, Zsombor I. Hegedűs, Zsófia Onódi, Alexandra Fábián, Attila Kovács, Tamás Radovits, Béla Merkely, Pál Pacher, Péter Ferdinandy, Zoltán V. Varga
GeroScience.2024;[Epub] CrossRef - Inhibition of visceral adipose tissue-derived pathogenic signals by activation of adenosine A2AR improves hepatic and cardiac dysfunction of NASH mice
Chia-Chang Huang, Hsiao-Yun Yeh, Roger Lin, Tsai-Ling Liao, Hsiao-Chin Shen, Ying-Ying Yang, Han-Chieh Lin
American Journal of Physiology-Gastrointestinal and Liver Physiology.2024; 326(4): G385. CrossRef - Is non-alcoholic fatty liver disease a sign of left ventricular diastolic dysfunction in patients with type 2 diabetes mellitus? A systematic review and meta-analysis
Sicheng Wang, Xiangyuan Zhang, Qiqi Zhang, Boxun Zhang, Linhua Zhao
BMJ Open Diabetes Research & Care.2023; 11(1): e003198. CrossRef - The effect of metabolic dysfunction-associated fatty liver disease and diabetic kidney disease on the risk of hospitalization of heart failure in type 2 diabetes: a retrospective cohort study
Seung Eun Lee, Juhwan Yoo, Bong-Seong Kim, Han Seok Choi, Kyungdo Han, Kyoung-Ah Kim
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(2): 220. CrossRef - Therapies for patients with coexisting heart failure with reduced ejection fraction and non-alcoholic fatty liver disease
Jose Arriola-Montenegro, Renato Beas, Renato Cerna-Viacava, Andres Chaponan-Lavalle, Karla Hernandez Randich, Diego Chambergo-Michilot, Herson Flores Sanga, Pornthira Mutirangura
World Journal of Cardiology.2023; 15(7): 328. CrossRef - Non-alcoholic Fatty Liver Disease and Its Association With Left Ventricular Diastolic Dysfunction: A Systematic Review
Namra V Gohil, Nida Tanveer, Vijaya Krishna Makkena, Arturo P Jaramillo, Babatope L Awosusi, Javaria Ayyub, Karan Nareshbhai Dabhi, Tuheen Sankar Nath
Cureus.2023;[Epub] CrossRef - Associations of advanced liver fibrosis with heart failure with preserved ejection fraction in type 2 diabetic patients according to obesity and metabolic goal achievement status
Wangyan Jiang, Zhelong Liu, Shaohua Liu, Tingting Du
Frontiers in Endocrinology.2023;[Epub] CrossRef - Non-Alcoholic Fatty Liver Disease and Echocardiographic Parameters of Left Ventricular Diastolic Function: A Systematic Review and Meta-Analysis
Athina Goliopoulou, Panagiotis Theofilis, Evangelos Oikonomou, Artemis Anastasiou, Panteleimon Pantelidis, Maria Ioanna Gounaridi, Georgios E. Zakynthinos, Ourania Katsarou, Eva Kassi, Vaia Lambadiari, Dimitris Tousoulis, Manolis Vavuranakis, Gerasimos Si
International Journal of Molecular Sciences.2023; 24(18): 14292. CrossRef - Non-alcoholic fatty liver disease and risk of cardiovascular diseases: clinical association, pathophysiological mechanisms, and management
Rong Yang, Jian-Gao Fan
Cardiology Plus.2023; 8(4): 217. CrossRef - Association of cardiovascular factors in diabetic patients with non-alcoholic fatty liver disease
Evangelos Cholongitas, Dimitrios Tsilingiris, Panagiota Diamantopoulou, Elpida Mastrogianni, Anastasios Tentolouris, Dimitrios Karagiannakis, Ioannis Moyssakis, George V. Papatheodoridis, Nikolaos Tentolouris
Hormones.2022; 21(1): 133. CrossRef - Non-alcoholic fatty liver disease association with structural heart, systolic and diastolic dysfunction: a meta-analysis
Jie Ning Yong, Cheng Han Ng, Chloe Wen-Min Lee, Yu Yi Chan, Ansel Shao Pin Tang, Margaret Teng, Darren Jun Hao Tan, Wen Hui Lim, Jingxuan Quek, Jieling Xiao, Yip Han Chin, Roger Foo, Mark Chan, Weiqin Lin, Mazen Noureddin, Mohammad Shadab Siddiqui, Mark D
Hepatology International.2022; 16(2): 269. CrossRef - Triglyceride and glucose index is a simple and easy‐to‐calculate marker associated with nonalcoholic fatty liver disease
Kyung‐Soo Kim, Sangmo Hong, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2022; 30(6): 1279. CrossRef - Association of Metabolic Dysfunction-Associated Fatty Liver Disease With Left Ventricular Diastolic Function and Cardiac Morphology
Dandan Peng, Zhenqiu Yu, Mingwei Wang, Junping Shi, Lei Sun, Yuanyuan Zhang, Wenbin Zhao, Chen Chen, Jiake Tang, Chunyi Wang, Jie Ni, Wen Wen, Jingjie Jiang
Frontiers in Endocrinology.2022;[Epub] CrossRef - NAFLD in Cardiovascular Diseases: A Contributor or Comorbidity?
Bing Chen, W.H. Wilson Tang, Mario Rodriguez, Kathleen E. Corey, Arun J. Sanyal, Patrick S. Kamath, Biykem Bozkurt, Hafeez Ul Hassan Virk, Gregg S. Pressman, Jeffrey V. Lazarus, Hashem B. El-Serag, Chayakrit Krittanawong
Seminars in Liver Disease.2022; 42(04): 465. CrossRef - Nonalcoholic fatty liver disease is associated with early left ventricular diastolic dysfunction in patients with type 2 diabeteS
Walaa Sheba, Eman Morsy, Salah Altahan, Mona Ayaad, Sameh A. Lashen
Alexandria Journal of Medicine.2022; 58(1): 117. CrossRef - Cardiac abnormalities in patients with nonalcoholic fatty liver disease
Yu Dong, Guangsen Li
Herz.2021; 46(2): 158. CrossRef - Elafibranor improves diet-induced nonalcoholic steatohepatitis associated with heart failure with preserved ejection fraction in Golden Syrian hamsters
François Briand, Julie Maupoint, Emmanuel Brousseau, Natalia Breyner, Mélanie Bouchet, Clément Costard, Thierry Leste-Lasserre, Mathieu Petitjean, Li Chen, Audrey Chabrat, Virgile Richard, Rémy Burcelin, Caroline Dubroca, Thierry Sulpice
Metabolism.2021; 117: 154707. CrossRef - Association of the Non‐Alcoholic Fatty Liver Disease Fibrosis Score with subclinical myocardial remodeling in patients with type 2 diabetes: A cross‐sectional study in China
Nengguang Fan, Xiaoying Ding, Qin Zhen, Liping Gu, Aifang Zhang, Tingting Shen, Yufan Wang, Yongde Peng
Journal of Diabetes Investigation.2021; 12(6): 1035. CrossRef - Nonalcoholic fatty liver disease, diastolic dysfunction, and impaired myocardial glucose uptake in patients with type 2 diabetes
Minyoung Lee, Kwang Joon Kim, Tae‐Ha Chung, Jaehyun Bae, Yong‐ho Lee, Byung‐Wan Lee, Bong‐Soo Cha, Mijin Yun, Eun Seok Kang
Diabetes, Obesity and Metabolism.2021; 23(4): 1041. CrossRef - Interplay between Heart Disease and Metabolic Steatosis: A Contemporary Perspective
Mohammad Said Ramadan, Vincenzo Russo, Gerardo Nigro, Emanuele Durante-Mangoni, Rosa Zampino
Journal of Clinical Medicine.2021; 10(8): 1569. CrossRef - Correlation Between 25-Hydroxyvitamin D Level and Cardiac Diastolic Dysfunction in Chinese Adults with Early-Onset Type 2 Diabetes Mellitus: A Cross-Sectional Study
Lei Xiu, Xiao-ai Yao, Tao Jiang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 1823. CrossRef - Bi-directional and temporal relationship between elevated alanine aminotransferase and hypertension in a longitudinal study of Chinese adults
Guoxin Huang, Hui Zhou, Chao Shen, Yihui Sheng, Ruyu Xue, Chen Dong, Shaoyan Zhang
Clinical and Experimental Hypertension.2021; 43(8): 750. CrossRef - Response: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (Diabetes Metab J 2020;44:267–76)
Hokyou Lee, Gyuri Kim, Yong-ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 486. CrossRef - Letter: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (Diabetes Metab J2020;44:267–76)
Sung Hoon Yu
Diabetes & Metabolism Journal.2020; 44(3): 482. CrossRef
- Anti-hepatopathy and anti-nephropathy activities of Taraxacum officinale in a rat model of Streptozotocin diabetes-induced hepatorenal toxicity and dyslipidemia via attenuation of oxidative stress, inflammation, apoptosis, electrolyte imbalances, and mito
- Obesity and Metabolic Syndrome
- Utility of Serum Albumin for Predicting Incident Metabolic Syndrome According to Hyperuricemia
- You-Bin Lee, Ji Eun Jun, Seung-Eun Lee, Jiyeon Ahn, Gyuri Kim, Jae Hwan Jee, Ji Cheol Bae, Sang-Man Jin, Jae Hyeon Kim
- Diabetes Metab J. 2018;42(6):529-537. Published online September 28, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0012
- 4,368 View
- 47 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Serum albumin and uric acid have been positively linked to metabolic syndrome (MetS). However, the association of MetS incidence with the combination of uric acid and albumin levels has not been investigated. We explored the association of albumin and uric acid with the risk of incident MetS in populations divided according to the levels of these two parameters.
Methods In this retrospective longitudinal study, 11,613 non-MetS participants were enrolled among 24,185 individuals who had undergone at least four annual check-ups between 2006 and 2012. The risk of incident MetS was analyzed according to four groups categorized by the sex-specific medians of serum albumin and uric acid.
Results During 55,407 person-years of follow-up, 2,439 cases of MetS developed. The risk of incident MetS increased as the uric acid category advanced in individuals with lower or higher serum albumin categories with hazard ratios (HRs) of 1.386 (95% confidence interval [CI], 1.236 to 1.554) or 1.314 (95% CI, 1.167 to 1.480). However, the incidence of MetS increased with higher albumin levels only in participants in the lower uric acid category with a HR of 1.143 (95% CI, 1.010 to 1.294).
Conclusion Higher levels of albumin were associated with an increased risk of incident MetS only in individuals with lower uric acid whereas higher levels of uric acid were positively linked to risk of incident MetS regardless of albumin level.
-
Citations
Citations to this article as recorded by- Dissecting the risk factors for hyperuricemia in vegetarians in Taiwan
Kai-Chieh Chang, Sin-Yi Huang, Wen-Hsin Tsai, Hao-Wen Liu, Jia-Sin Liu, Chia-Lin Wu, Ko-Lin Kuo
Journal of the Chinese Medical Association.2024; 87(4): 393. CrossRef - A predictive model for hyperuricemia among type 2 diabetes mellitus patients in Urumqi, China
Palizhati Abudureyimu, Yuesheng Pang, Lirun Huang, Qianqian Luo, Xiaozheng Zhang, Yifan Xu, Liang Jiang, Patamu Mohemaiti
BMC Public Health.2023;[Epub] CrossRef - Synergistic Interaction between Hyperuricemia and Abdominal Obesity as a Risk Factor for Metabolic Syndrome Components in Korean Population
Min Jin Lee, Ah Reum Khang, Yang Ho Kang, Mi Sook Yun, Dongwon Yi
Diabetes & Metabolism Journal.2022; 46(5): 756. CrossRef - Nutritional Biomarkers and Heart Rate Variability in Patients with Subacute Stroke
Eo Jin Park, Seung Don Yoo
Nutrients.2022; 14(24): 5320. CrossRef - Mean and visit-to-visit variability of glycemia and left ventricular diastolic dysfunction: A longitudinal analysis of 3025 adults with serial echocardiography
Jiyeon Ahn, Janghyun Koh, Darae Kim, Gyuri Kim, Kyu Yeon Hur, Sang Won Seo, Kyunga Kim, Jae Hyeon Kim, Jeong Hoon Yang, Sang-Man Jin
Metabolism.2021; 116: 154451. CrossRef - Can biomarkers be used to improve diagnosis and prediction of metabolic syndrome in childhood cancer survivors? A systematic review
Vincent G. Pluimakers, Selveta S. van Santen, Marta Fiocco, Marie‐Christine E. Bakker, Aart J. van der Lelij, Marry M. van den Heuvel‐Eibrink, Sebastian J. C. M. M. Neggers
Obesity Reviews.2021;[Epub] CrossRef - Heart Disease and Stroke Statistics—2020 Update: A Report From the American Heart Association
Salim S. Virani, Alvaro Alonso, Emelia J. Benjamin, Marcio S. Bittencourt, Clifton W. Callaway, April P. Carson, Alanna M. Chamberlain, Alexander R. Chang, Susan Cheng, Francesca N. Delling, Luc Djousse, Mitchell S.V. Elkind, Jane F. Ferguson, Myriam Forn
Circulation.2020;[Epub] CrossRef - Association between dairy product consumption and hyperuricemia in an elderly population with metabolic syndrome
Guillermo Mena-Sánchez, Nancy Babio, Nerea Becerra-Tomás, Miguel Á. Martínez-González, Andrés Díaz-López, Dolores Corella, Maria D. Zomeño, Dora Romaguera, Jesús Vioque, Ángel M. Alonso-Gómez, Julia Wärnberg, José A. Martínez, Luís Serra-Majem, Ramon Estr
Nutrition, Metabolism and Cardiovascular Diseases.2020; 30(2): 214. CrossRef - Evaluation of serum uric acid levels in patients with rosacea
Nermin Karaosmanoglu, Engin Karaaslan, Pınar Ozdemir Cetinkaya
Archives of Dermatological Research.2020; 312(6): 447. CrossRef - Letter: Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study (Diabetes Metab J 2019;43:521-9)
Jin Hwa Kim
Diabetes & Metabolism Journal.2019; 43(5): 727. CrossRef
- Dissecting the risk factors for hyperuricemia in vegetarians in Taiwan
- Epidemiology
-
- High Proportion of Adult Cases and Prevalence of Metabolic Syndrome in Type 1 Diabetes Mellitus Population in Korea: A Nationwide Study
- You-Bin Lee, Kyungdo Han, Bongsung Kim, Sang-Man Jin, Seung-Eun Lee, Ji Eun Jun, Jiyeon Ahn, Gyuri Kim, Jae Hyeon Kim
- Diabetes Metab J. 2019;43(1):76-89. Published online August 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0048
- 5,861 View
- 109 Download
- 26 Web of Science
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background The prevalence and incidence of type 1 diabetes mellitus (T1DM) in all age groups and the prevalence of metabolic syndrome in patients with T1DM in Korea were estimated.
Methods The incidence and prevalence of T1DM between 2007 and 2013 were calculated using the Korean National Health Insurance Service (NHIS) datasets of claims. Clinical characteristics and prevalence of metabolic syndrome in individuals with T1DM between 2009 and 2013 were determined using the database of NHIS preventive health checkups.
Results The prevalence of T1DM in Korea between 2007 and 2013 was 0.041% to 0.047%. The annual incidence rate of T1DM in Korea in 2007 to 2013 was 2.73 to 5.02/100,000 people. Although the incidence rate of typical T1DM was highest in teenagers, it remained steady in adults over 30 years of age. In contrast, the incidence rate of atypical T1DM in 2013 was higher in people aged 40 years or older than in younger age groups. Age- and sex-adjusted prevalence of metabolic syndrome in patients with T1DM was 51.65% to 55.06% between 2009 and 2013.
Conclusion T1DM may be more common in Korean adults than previously believed. Metabolic syndrome may be a frequent finding in individuals with T1DM in Korea.
-
Citations
Citations to this article as recorded by- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes & Metabolism.2024; 50(1): 101505. CrossRef - Incidence and trends of type 1 diabetes before and after 2000 in the Western Pacific Region: A systematic review and meta-analysis
Du Wang, Xiaoli Hou, Juan Huang, Jianjing Sun, Takashi Kadowaki, Moon-Kyu Lee, Alicia J. Jenkins, Linong Ji
Diabetes Research and Clinical Practice.2024; 207: 111055. CrossRef - The emergence of obesity in type 1 diabetes
Martin T. W. Kueh, Nicholas W. S. Chew, Ebaa Al-Ozairi, Carel W. le Roux
International Journal of Obesity.2024; 48(3): 289. CrossRef - Prevalence of Metabolic Syndrome and Its Risk Factors Influence on Microvascular Complications in Patients With Type 1 and Type 2 Diabetes Mellitus
Asad Riaz, Shoaib Asghar, Salman Shahid, Haider Tanvir, Muhammad Hamza Ejaz, Mamuna Akram
Cureus.2024;[Epub] CrossRef - Risk of Depression according to Cumulative Exposure to a Low-Household Income Status in Individuals with Type 2 Diabetes Mellitus: A Nationwide Population- Based Study
So Hee Park, You-Bin Lee, Kyu-na Lee, Bongsung Kim, So Hyun Cho, So Yoon Kwon, Jiyun Park, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Kyungdo Han, Jae Hyeon Kim
Diabetes & Metabolism Journal.2024; 48(2): 290. CrossRef - Comparison of Insulin-Treated Patients with Ambiguous Diabetes Type with Definite Type 1 and Type 2 Diabetes Mellitus Subjects: A Clinical Perspective
Insa Laspe, Juris J. Meier, Michael A. Nauck
Diabetes & Metabolism Journal.2023; 47(1): 140. CrossRef - Clinical and biochemical profile of childhood–adolescent-onset type 1 diabetes and adult-onset type 1 diabetes among Asian Indians
Viswanathan Mohan, Ganesan Uma Sankari, Anandakumar Amutha, Ranjit Mohan Anjana, Saravanan Jeba Rani, Ranjit Unnikrishnan, Ulagamathesan Venkatesan, Coimbatore Subramanian Shanthi Rani
Acta Diabetologica.2023; 60(4): 579. CrossRef - Subtypes of type 2 diabetes and their association with outcomes in Korean adults - A cluster analysis of community-based prospective cohort
You-Cheol Hwang, Hong-Yup Ahn, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
Metabolism.2023; 141: 155514. CrossRef - Insulin Fact Sheet in Type 1 and 2 Diabetes Mellitus and Trends of Antidiabetic Medication Use in Insulin Users with Type 2 Diabetes Mellitus: 2002 to 2019
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(2): 211. CrossRef - Insulin resistance is more frequent in type 1 diabetes patients with long disease duration
Yuting Xie, Mei Shi, Xiaolin Ji, Fansu Huang, Li Fan, Xia Li, Zhiguang Zhou
Diabetes/Metabolism Research and Reviews.2023;[Epub] CrossRef - Long-term Effectiveness of the National Diabetes Quality Assessment Program in South Korea
Ji Hye Huh, Serim Kwon, Gui Ok Kim, Bo Yeon Kim, Kyoung Hwa Ha, Dae Jung Kim
Diabetes Care.2023; 46(9): 1700. CrossRef - Low Household Income Status and Death from Pneumonia in People with Type 2 Diabetes Mellitus: A Nationwide Study
You-Bin Lee, So Hee Park, Kyu-na Lee, Bongsung Kim, So Yoon Kwon, Jiyun Park, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Kyungdo Han, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(5): 682. CrossRef - Impact of statin treatment on cardiovascular risk in patients with type 1 diabetes: a population-based cohort study
Joonsang Yoo, Jimin Jeon, Minyoul Baek, Sun Ok Song, Jinkwon Kim
Journal of Translational Medicine.2023;[Epub] CrossRef - Association between Metabolic Syndrome and Microvascular Complications in Chinese Adults with Type 1 Diabetes Mellitus
Qianwen Huang, Daizhi Yang, Hongrong Deng, Hua Liang, Xueying Zheng, Jinhua Yan, Wen Xu, Xiangwen Liu, Bin Yao, Sihui Luo, Jianping Weng
Diabetes & Metabolism Journal.2022; 46(1): 93. CrossRef - The Incidence of Adult-Onset Type 1 Diabetes: A Systematic Review From 32 Countries and Regions
Jessica L. Harding, Pandora L. Wander, Xinge Zhang, Xia Li, Suvi Karuranga, Hongzhi Chen, Hong Sun, Yuting Xie, Richard A. Oram, Dianna J. Magliano, Zhiguang Zhou, Alicia J. Jenkins, Ronald C.W. Ma
Diabetes Care.2022; 45(4): 994. CrossRef - Age at Diagnosis and the Risk of Diabetic Nephropathy in Young Patients with Type 1 Diabetes Mellitus
Jong Ha Baek, Woo Je Lee, Byung-Wan Lee, Soo Kyoung Kim, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim
Diabetes & Metabolism Journal.2021; 45(1): 46. CrossRef - Genomic ancestry and metabolic syndrome in individuals with type 1 diabetes from an admixed population: a multicentre, cross‐sectional study in Brazil
B. S. V. Barros, D. C. Santos, L. G. N. Melo, M. H. Pizarro, L. H. Muniz, D. A. Silva, L. C. Porto, M. B. Gomes
Diabetic Medicine.2021;[Epub] CrossRef - The Interplay Between Diet and the Epigenome in the Pathogenesis of Type-1 Diabetes
Amira Kohil, Maha Al-Asmakh, Mashael Al-Shafai, Annalisa Terranegra
Frontiers in Nutrition.2021;[Epub] CrossRef - Risk of early mortality and cardiovascular disease according to the presence of recently diagnosed diabetes and requirement for insulin treatment: A nationwide study
You‐Bin Lee, Kyungdo Han, Bongsung Kim, Min Sun Choi, Jiyun Park, Minyoung Kim, Sang‐Man Jin, Kyu Yeon Hur, Gyuri Kim, Jae Hyeon Kim
Journal of Diabetes Investigation.2021; 12(10): 1855. CrossRef - Age at Diagnosis and the Risk of Diabetic Nephropathy in Young Patients with Type 1 Diabetes Mellitus (Diabetes Metab J 2021;45:46-54)
Ye Seul Yang, Tae Seo Sohn
Diabetes & Metabolism Journal.2021; 45(2): 277. CrossRef - Comparison of fracture risk between type 1 and type 2 diabetes: a comprehensive real-world data
J. Ha, C. Jeong, K.-D. Han, Y. Lim, M.K. Kim, H.-S. Kwon, K.-H. Song, M.I. Kang, K.-H. Baek
Osteoporosis International.2021; 32(12): 2543. CrossRef - Early mortality and cardiovascular disease, varied association with body mass index and its changes in insulin-treated diabetes: a nationwide study
You-Bin Lee, Bongsung Kim, Jiyun Park, Minyoung Kim, Min Sun Choi, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Kyungdo Han, Jae Hyeon Kim
International Journal of Obesity.2021; 45(11): 2482. CrossRef - Young-onset type 2 diabetes in South Korea: a review of the current status and unmet need
Ye Seul Yang, Kyungdo Han, Tae Seo Sohn, Nam Hoon Kim
The Korean Journal of Internal Medicine.2021; 36(5): 1049. CrossRef - Positive association between the ratio of triglycerides to high-density lipoprotein cholesterol and diabetes incidence in Korean adults
Joungyoun Kim, Sang-Jun Shin, Ye-Seul Kim, Hee-Taik Kang
Cardiovascular Diabetology.2021;[Epub] CrossRef - Mortality and causes of death in a population with blindness in Korea: A longitudinal follow-up study using a national sample cohort
Hyo Geun Choi, Min Joung Lee, Sang-Mok Lee
Scientific Reports.2020;[Epub] CrossRef - Hospitalization for heart failure incidence according to the transition in metabolic health and obesity status: a nationwide population-based study
You-Bin Lee, Da Hye Kim, Seon Mee Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Yong Gyu Park, Kyungdo Han, Hye Jin Yoo
Cardiovascular Diabetology.2020;[Epub] CrossRef - Management of Type 1 Diabetes Mellitus in Adults
Hye Ryoung Yun
The Journal of Korean Diabetes.2020; 21(3): 156. CrossRef - New Insulin Pumps and Open Source Artificial Pancreas System in Korea
Jae Hyeon Kim
The Journal of Korean Diabetes.2020; 21(4): 197. CrossRef - Risk of early mortality and cardiovascular disease in type 1 diabetes: a comparison with type 2 diabetes, a nationwide study
You-Bin Lee, Kyungdo Han, Bongsung Kim, Seung-Eun Lee, Ji Eun Jun, Jiyeon Ahn, Gyuri Kim, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2019;[Epub] CrossRef - Risk of end‐stage renal disease from chronic kidney disease defined by decreased glomerular filtration rate in type 1 diabetes: A comparison with type 2 diabetes and the effect of metabolic syndrome
You‐Bin Lee, Kyungdo Han, Bongsung Kim, Ji Eun Jun, Seung‐Eun Lee, Jiyeon Ahn, Gyuri Kim, Sang‐Man Jin, Jae Hyeon Kim
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef
- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study

 KDA
KDA
 First
First Prev
Prev





